How to Talk About Bedwetting Without Shame or Embarrassment
If your child wets the bed, the topic can feel awkward, uncomfortable—even taboo. It’s a conversation no one wants to have, but one that needs to happen if we want children to grow up feeling confident, secure, and supported.
So how do you talk about bedwetting without making your child feel ashamed or embarrassed?
Whether your child is 6 or 16, this guide will help you open up the conversation in a way that builds trust, preserves their dignity, and helps them feel safe—even on the hardest nights.
💬
Why Language Around Bedwetting Matters
Bedwetting (nocturnal enuresis) is a deeply personal issue, and how we talk about it shapes how a child feels about themselves.
Unfortunately, most children:
- Feel ashamed
- Worry that something is wrong with them
- Are afraid of being discovered by friends or siblings
- May interpret adult frustration as disappointment or blame
The good news?
Parents have enormous power to change the emotional tone surrounding bedwetting—starting with how you talk about it.
❌
Common Phrases That Accidentally Shame Children
Without meaning to, even well-meaning parents can make bedwetting feel like a moral failure or personal flaw.
Here are some examples to avoid:
| 🚫 What You Might Say | 🧠 What Your Child Might Hear |
|---|---|
| “You’re too old for this.” | “There’s something wrong with me.” |
| “Why did you do this again?” | “I did it on purpose.” |
| “We’ve talked about this!” | “I’m not allowed to have accidents.” |
| “Can’t you just get up and go?” | “Everyone else can but I can’t—what’s wrong with me?” |
| “This is disgusting.” | “I’m disgusting.” |
Even if said in frustration, these comments stick—and can lead to long-term issues with self-esteem, secrecy, or anxiety.
✅
What to Say Instead: Supportive Alternatives
Language that normalizes, reassures, and shows unconditional love helps your child stay open and engaged.
| ✅ Try Saying This… | 🧠 What It Teaches |
|---|---|
| “This happens to lots of kids your age.” | “I’m not alone.” |
| “Your body is still learning. That’s okay.” | “It’s not my fault.” |
| “We’ll get through this together.” | “I’m supported.” |
| “Thanks for helping clean up. That was mature.” | “I can take responsibility, not blame.” |
| “Wet or dry, I love you just the same.” | “My worth doesn’t depend on this.” |
The key is to make bedwetting no bigger a deal than it needs to be—not ignored, not dramatized, just part of the routine.
👂
How to Start the Conversation
Don’t wait for the “perfect” time.
Start small, speak gently, and follow your child’s lead.
For younger kids:
“Sometimes our bodies take longer to learn how to stay dry at night. It’s normal, and we’ll figure it out together.”
For older kids or teens:
“I know this is something that might feel embarrassing, but I want you to know there’s nothing wrong with you. I’m here to help however you need.”
Make eye contact, speak softly, and keep your tone matter-of-fact. Avoid big emotional swings—they may make your child feel like they’ve done something terribly wrong.
🛑
What If They Don’t Want to Talk About It?
That’s okay. Let them know:
- You’re always available if they want to talk
- You’ll continue to support them whether or not they feel ready to chat
- Their privacy will be respected
Try:
“You don’t have to talk about it if you don’t want to. Just know I’m here, and we can figure things out as a team.”
Children often open up on their own timeline—especially when they know you’re safe and pressure-free.
🧒
Helping Your Child Understand What’s Happening
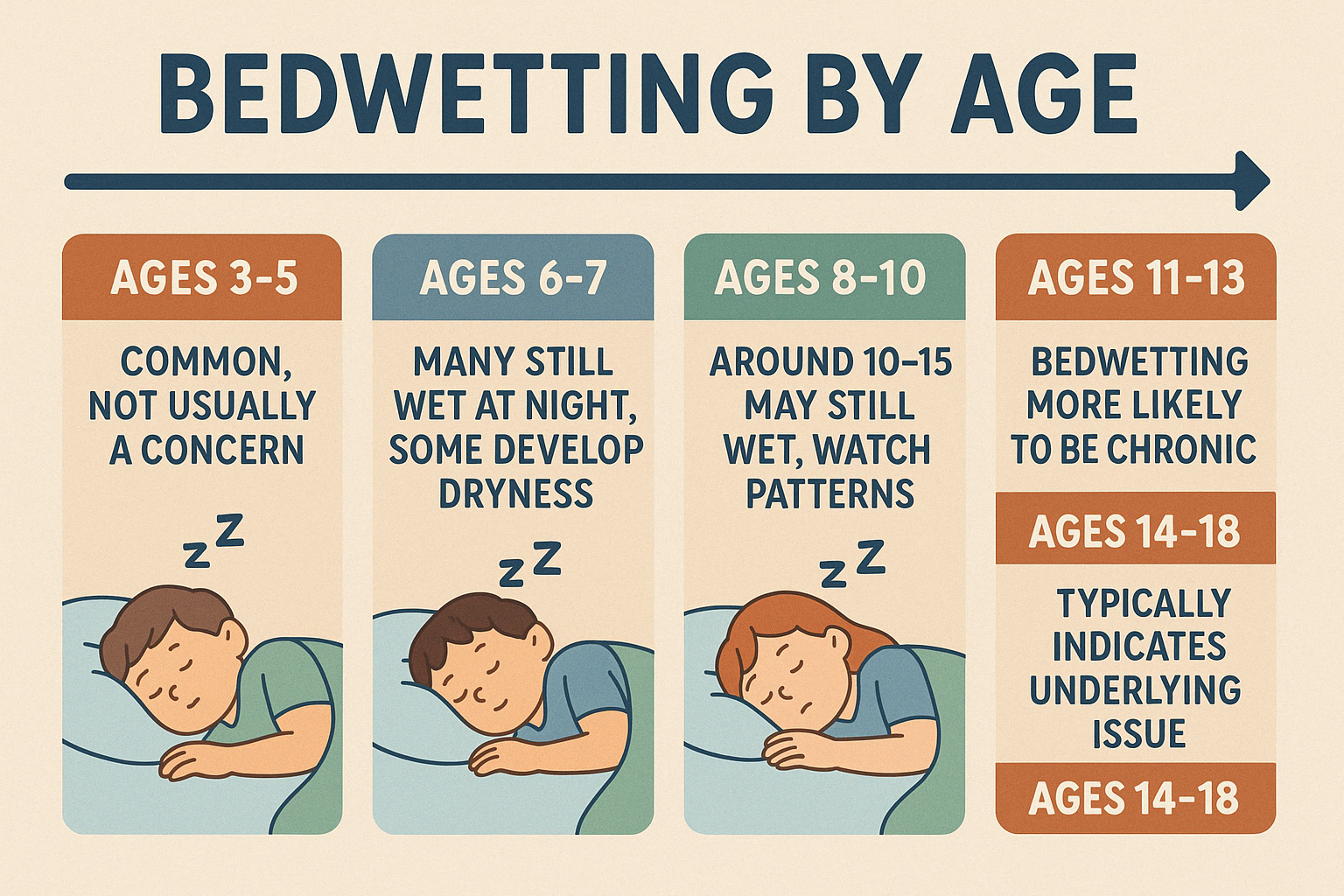
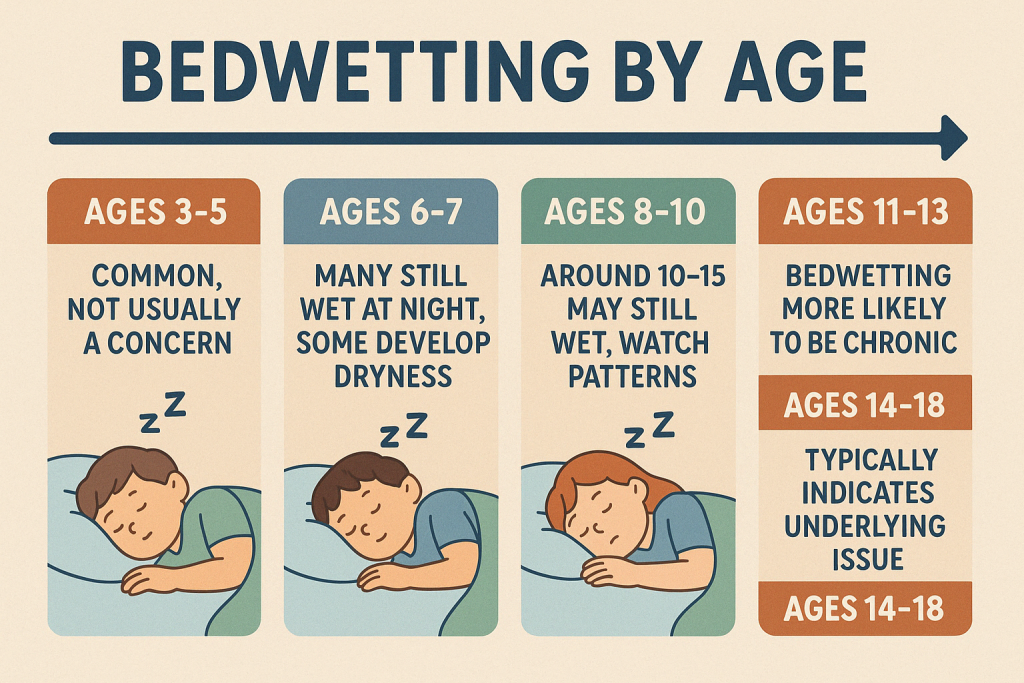
Many children (especially between ages 6–10) need help understanding why bedwetting happens.
Age-appropriate explanations:
- “Your brain and bladder aren’t waking up together just yet, but they will.”
- “Some people sleep so deeply, they don’t notice when they need the toilet.”
- “It’s not something you can just choose to stop—your body is still growing.”
Reinforce that:
- They are not broken.
- They are not dirty.
- They are not doing anything wrong.
Bonus: Share stories of family members who also wet the bed. This makes the experience feel less isolating and more normal.
🛏
Talking About Clean-Up Without Adding Pressure
If your child is old enough to help with clean-up, involve them—but frame it as practical, not punishment.
Say:
“Let’s grab the new sheets and pajamas together—thanks for being part of the solution.”
Avoid:
- “You made this mess—you clean it up.”
- “This is your fault—you fix it.”
Instead, treat clean-up as part of the process—no drama, no shame, just life.
This builds resilience and responsibility, not guilt.
👪
What About Talking to Siblings or Other Family Members?
Privacy is key. You don’t want your child to feel “outed” or humiliated.
Tips:
- Only tell siblings on a need-to-know basis (e.g., shared rooms).
- Use neutral language: “Sometimes their body doesn’t wake up for the toilet yet. It’s not a big deal.”
- Set firm boundaries: No teasing allowed. Ever.
- Praise siblings who respect privacy and support without judgement.
Let your child decide what they’re comfortable with others knowing.
🗣️
Talking to Teachers, GPs, or Sleepover Hosts
When it’s necessary to involve other adults, model respectful, discrete communication.
Talk to your child first:
“We might need to tell the school nurse just so they can help you if there’s ever an issue. We’ll do it in a way that feels okay to you.”
Let them be part of the decision whenever possible.
If speaking to a teacher, club leader, or friend’s parent:
- Stick to essentials
- Avoid emotional language
- Emphasize confidence and normalcy
Example:
“My son sometimes has accidents at night. He uses protective products and is very independent, but I wanted to let you know in case he ever needs support.”
🧠
The Long-Term Power of Shame-Free Communication
Children who grow up feeling safe to talk about bedwetting:
- Are less likely to develop anxiety around sleep
- Build greater resilience and self-trust
- Are more open to trying solutions like alarms or medications
- Recover more quickly emotionally when the issue resolves
Even if the bedwetting lasts into the teen years, shame-free children are:
- More independent
- More likely to manage hygiene themselves
- Better at protecting their own dignity in social settings
🛑
What If You’ve Already Said the “Wrong” Thing?
It’s never too late to repair.
Try:
“I’m sorry I got frustrated before. I know this isn’t something you’re doing on purpose, and I want to do better at helping you feel safe.”
Owning your words doesn’t make you weak. It makes your child feel seen, respected, and loved.
Repair is more powerful than perfection.
🛠
Conversation Starters by Age Group
Here are a few examples of gentle openers that create space:
Ages 4–6:
- “Oops! That happens sometimes. Let’s get you cleaned up.”
- “Your body’s still learning! You’ll get there.”
Ages 7–10:
- “I know you’re trying. This isn’t about effort—it’s just something lots of kids deal with.”
- “Would you like to try a new bedtime routine to help?”
Ages 11–13:
- “This might feel private, but you don’t have to go through it alone.”
- “Want to talk about ways to make this easier for you?”
Teens (14+):
- “I totally respect your privacy. Just know there are options if you ever want to try something new.”
- “Would you prefer to handle it yourself, or want support?”
Always adapt to your child’s personality—but lead with dignity, not diagnosis.
✨ Final Thoughts: Your Words Can Heal
Bedwetting is a medical issue, not a moral one.
How you talk about it shapes how your child talks to themselves.
In your home, bedwetting should be:
- Just a thing that happens
- A challenge, not a character flaw
- Something they can talk about, not hide from
You don’t need to solve it overnight. But you can make it feel safe.
Because ultimately, it’s not about sheets or alarms—it’s about connection.
And that starts with one shame-free conversation at a time.